Intro: Gallbladder Bloating After Surgery
Gallbladder bloating is a predominant issue, particularly for people who have gone through gallbladder surgery. This uneasiness can be confusing, and disentangling the causes and associations of bloating becomes fundamental for viable postoperative administration and the early recognition of potential gallbladder bloating and other issues. Does gallbladder cause bloating?
The Importance of the Gallbladder:
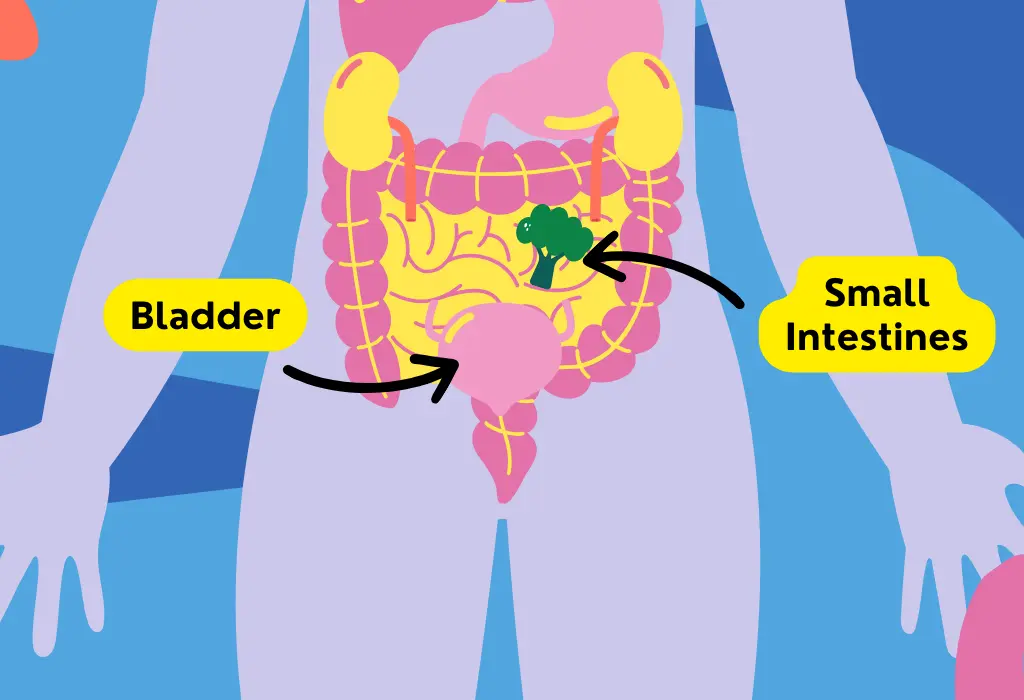
The gallbladder has a fundamental job in the digestive system as a reservoir for bile created by the liver. Bile is an essential digestive liquid that aids in separating and absorbing fats from our food. When we eat, the gallbladder contracts, releasing bile into the small intestine to work with the digestion of fats.
- Significance in Digestion: The gallbladder’s commitment to digestion is necessary, ensuring that fats are successfully processed and nutrients are absorbed. Disturbances in this process can prompt malabsorption, influencing general digestive well-being.
- Bile Storage and Release: The gallbladder’s capacity to store and release bile as required is a finely tuned mechanism. After gallbladder surgery, this mechanism undergoes a significant change. With the gallbladder eliminated, bile flows straightforwardly from the liver into the small intestine, resulting in a continuous, less controlled release.
- Influence on Digestive Wellbeing: Disturbances in the gallbladder’s ordinary working can have cascading effects on the digestive system. Bloating can arise when the digestive process is disrupted, and the body struggles to adjust to the absence of the gallbladder.
- Connection to Bloating: does the gallbladder cause bloating; it may happen because of various factors connected with the gallbladder. Without the gallbladder’s guidelines, the continuous progression of bile can overpower the digestive system, prompting bloating, gas, and discomfort. Furthermore, adjusting bile composition and release procedure post-surgery can add to digestive disturbances.
Bloating After Gallbladder Surgery: Understanding the Causes and Adjustments
Gallbladder surgery, frequently a cholecystectomy, is a standard strategy pointed toward mitigating issues like gallstones. Nonetheless, numerous individuals experience gallbladder bloating after surgery, raising questions about the reasons behind this discomfort and the body’s transformation to the absence of the gallbladder.
Reasons Behind Bloating:
1. Changed Bile Stream: Post-gallbladder surgery, there is an outstanding shift in how bile is overseen inside the digestive system. Bile streams constantly from the liver into the small intestine without the gallbladder as a storage reservoir. This adjustment of bile release can overpower the digestive system, adding to gallbladder bloating.
2. Continuous Bile Dribble: The gallbladder acts as a regulator, releasing gathered bile in response to food consumption. Without this guideline, the constant bile trickle can prompt unfortunate fat digestion, causing bloating, gas, and discomfort.
3. Changes in Bile Composition: The composition of bile can also be modified after gallbladder removal. The absence of the gallbladder might result in a less focused and less compelling bile, influencing the breakdown of fats and general digestion.
Distinguishing Gallbladder Bloating: Perceiving Symptoms and Affirming Diagnosis
Bloating connected with gallbladder issues manifests through specific symptoms and signs. Perceiving these indicators is crucial for ideal diagnosis and viable administration. Here is an outline:
Symptoms and Signs of Gallbladder Bloating:
Post-Feast Discomfort: Bloating often occurs after meals, especially those high in fat. The body’s struggle to digest fats without the gallbladder can prompt a sensation of fullness and discomfort.
Stomach Distension: Individuals might see an increased stomach size, often joined by a tight or swollen sensation. This can be a result of gas gathering because of wasteful fat digestion.
Fart and Burping: Excessive gas creation in response to inadequately digested fats can increase fart and burping. These symptoms are demonstrative of digestive irregularity.
Irregular feces release: Shifts in gut rituals, such as runs or constipation, may accompany gallbladder bloating. The irregularities stem from the disruption of bile release, influenced by extensive digestion.
Upper Stomach Torment: Discomfort or less than overwhelming torment in the upper stomach locale, especially on the right side, is a typical symptom. This can be credited to the modified bile stream and digestion processes.
Statistics on Bloating after Gallbladder Surgery
Commonness:
Bloating is a typical grievance after gallbladder surgery, known as cholecystectomy. Numerous patients might encounter bloating or discomfort in the postoperative period.
Timelines for Postoperative Bloating:
- Quick Postoperative Period: Some patients might encounter bloating instantly after surgery because of the consequences of anaesthesia, surgical injury, and the presentation of gas into the stomach cavity during laparoscopic procedures.
- First Couple of Days: Bloating is usually detailed in the first couple of days following surgery as the body adjusts to the absence of the gallbladder and adapts to changes in the bile stream and digestion.
- Weeks to Months: By and large, bloating tends to work over the weeks to months following surgery as the body adapts to the changes.
Variations in Individual Experiences:
- Sort of Surgery: The strategy for gallbladder removal (laparoscopic or open surgery) can impact the degree of postoperative bloating.
- Individual Physiology: Every person’s body reacts contrastingly to surgery, and factors such as age well-being, and exceptional physiology can add to variations in postoperative experiences.
- Dietary Choices: Dietary habits and choices post-surgery can influence digestive symptoms, including bloating.
The administration and Comfort:
- Dietary Modifications: Patients are often advised to roll out continuous nutritional improvements, such as keeping away from greasy foods and slowly introducing them again.
- Physical Movement: Delicate physical action can help with digestion and decrease bloating.
- Clinical Counsel: Patients must adhere to postoperative consideration instructions given by their medical care providers and seek a clinical appeal if symptoms persist or worsen.
Gallbladder Disease and Bloating:
Gallbladder diseases, including gallstones and aggravation (cholecystitis), can add to digestive disturbances and bloating. Here is an assessment of the relationship:
Gallstones:
- Obstruction of Bile Stream: Gallstones can block the usual bile stream from the gallbladder to the small intestine. This obstruction can prompt a reinforcement of bile, causing discomfort and bloating.
- Aggravation and Bothering: Gallstones might cause irritation and disturbance of the gallbladder, compounding digestive symptoms such as bloating.
- Cholecystitis (inflammation of the Gallbladder): inflammation-induced Disturbances: Irritation in the gallbladder can prompt disturbances in the ordinary digestive process, resulting in bloating.
- Weakened Bile Storage and Release: The gallbladder’s capability stores bile and releases it in response to ingesting greasy foods. Aggravation can weaken these functions, influencing digestion and causing bloating.
Digestive Disturbances:
- Modified Bile Composition: Gallbladder diseases can change the composition of bile, influencing its capacity to emulsify fats. This can prompt difficulties in fat digestion, adding to bloating.
- Changes in Stomach Microbiota: Digestive disturbances associated with gallbladder diseases might impact the composition of the stomach microbiota, possibly adding to bloating.
Dietary Strategies for Gallbladder Bloating Management:
Post-Surgery Dietary Adjustments:
- Progressive introduction of Fats: Patients are often advised to introduce fats into their eating regimen once again after gallbladder surgery. This helps the body adjust to the absence of the gallbladder and minimizes digestive discomfort, including bloating.
- Small, Incessant Meals: Feasting on smaller, more successive meals rather than enormous, weighty meals can help oversee bloating by decreasing the heap on the digestive system.
Dietary Considerations for Gallbladder bloating and Other Issues:
- Low-Fat Eating Routine: For individuals with gallbladder diseases, incorporating those with gallstones or irritation, a low-fat eating regimen is often prescribed to limit the responsibility on the digestive system and diminish the risk of setting off symptoms like gallbladder bloating.
- High-Fiber Foods: Fiber-rich foods can help digestion and advance inside consistency. Nonetheless, individual tolerance to fibre varies, so it’s essential to monitor its effects on gallbladder surgery.
- Hydration: Legitimate hydration is urgent for digestive wellbeing. It helps keep up with normal defecations and can mitigate bloating.
Conclusion:
Gallbladder diseases like gallstones and aggravation can add to digestive disturbances and gallbladder bloating. Gallstones might obstruct the bile stream, prompting discomfort and bloating, while aggravation can hinder the gallbladder’s typical functions, affecting digestion. Postoperative bloating after gallbladder surgery is normal, and proactive management is critical. Progressive dietary adjustments, including the presentation of fats and the reception of a low-fat eating regimen, are vital in limiting gallbladder bloating. Individuals are advised to consult medical care professionals for personalized direction, as responses to dietary changes can differ. Seeking clinical guidance is principal for persistent or worsening symptoms; it is instantly addressed to ensure that any hidden issues are addressed.
A holistic way to deal with digestive well-being is essential for individuals, regardless of gallbladder bloating. Keeping a reasonable eating regimen, staying hydrated, and integrating probiotics can improve general digestive prosperity. Those without gallbladders should embrace careful eating practices to support digestion. In contrast, individuals with gallbladder issues should work closely with medical services professionals to fit dietary plans for their needs. Emphasizing the importance of individualized care and ordinary clinical check-ups, this holistic methodology aims to upgrade general digestive well-being, fostering a proactive mindset towards prosperity.
References:
Colecchia, A., Sandri, L., Staniscia, T., Vestito, A., Capodicasa, S., Portincasa, P., Mazzella, G., Roda, E., & Festi, D. (2003). Gallbladder motility and functional gastrointestinal disorders. Digestive and Liver Disease, 35, 30–34.
Europe PMC. (n.d.). Europe PMC.
Heffernon, E. W. (1960). IRRITABLE COLON AND GALLBLADDER DISEASE. Journal of the American Medical Association.
Ros, E., & Zambón, D. (1987). Postcholecystectomy symptoms. A prospective study of gall stone patients before and two years after surgery. Gut, 28(11), 1500–1504.




